By Tracy Beanz & Michelle Edwards
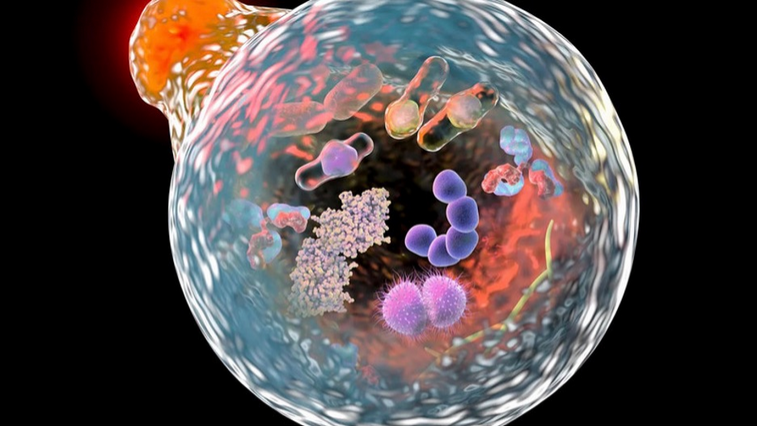
It cannot be articulated enough that the glorious human body that we are immensely blessed to inhabit is created to clean, heal, and repair itself when needed. One such incredible way is through our body’s natural process of cellular cleanup and repair, known as autophagy, which is akin to a cleaning crew inside the body’s cells. Autophagy, which means “self-eating,” enables our cells to break down and recycle their damaged or worn-out components, removing toxic buildup and preparing the stage for cellular renewal. New research indicates that while autophagy becomes increasingly consequential with age, it also slows down with age. However, there is also good news. The study found that certain practices, such as fasting and exercising, can help stimulate the natural process of autophagy even later in life as we age. Pretty incredible.
Indeed, though complicated, at the basic level, the natural process of autophagy breaks down and removes damaged or unnecessary toxins in our cells to keep them healthy. The cellular cleanup process affects CD8 T cells, which are key immune cells that fight infections and diseases by attacking infected or cancerous cells. The study, titled “Autophagy repression by antigen and cytokines shapes mitochondrial, migration, and effector machinery in CD8 T cells,” demonstrates, not surprisingly, that autophagy is critical for the proper function of CD8 T cells. It enables these cells to maintain healthy mitochondria (the energy factory of cells), supports their ability to move around the body, and ensures they can effectively fight off threats. The research highlights how autophagy is influenced by external signals, such as antigens (molecules that trigger immune responses) and cytokines (proteins that regulate immune activity).
So, how do antigens and cytokines affect autophagy? According to the study, specific signals, such as pro-inflammatory cytokines, can suppress autophagy in CD8 T cells. This means that when these cells are activated to fight an infection, their cleanup process slows down. Using special tools to measure how autophagy changes in these cells over 24 hours, the researchers found that, unlike pro-inflammatory cytokines, memory cytokines (which help T cells “remember” past infections) don’t appear to reduce autophagy. The researchers noted that this difference suggests that autophagy levels vary depending on whether the immune system is in an active fighting mode or a resting, memory-forming mode.
The study also explores how nutrients control autophagy in CD8 T cells. For example, when cells lack amino acids or are treated with the drug rapamycin (a drug used for organ transplant rejection and anti-aging), a protein complex known as mTORC1 (which normally promotes cell growth) is inhibited, thereby boosting autophagy. However, glucose deprivation, which activates another protein called AMPK, does not trigger autophagy in these cells. This indicates that autophagy in CD8 T cells is specifically sensitive to certain nutrient signals, such as amino acid availability, but not others, like glucose levels. This finding is significant because it reveals how the cell’s environment can fine-tune its cleanup process.
When autophagy is blocked (for example, by inhibiting a protein called VPS34), CD8 T cells accumulate damaged mitochondria, which can harm their ability to function correctly. The study also found that autophagy helps remove proteins associated with cell death, thereby promoting T-cell survival. This action is crucial because healthy CD8 T cells must survive and move effectively to combat infections or tumors. By clearing out damaged parts, autophagy supports the cells’ energy production, movement, and overall effectiveness as part of the immune system.
While quite complicated, the research suggests that controlling autophagy could improve how CD8 T cells function, thus potentially leading to better immune responses against diseases like infections or cancer. Indeed, by better understanding how signals like cytokines and nutrients affect autophagy, it stands to reason that scientists will—with a likely hefty profit in mind—develop new treatments to enhance T-cell function. There is already a considerable online market for the sale of rapamycin, which, again, boosts autophagy with the hope of helping immune cells stay healthy and effective. But hold on a minute. Since autophagy is a function of a naturally healthy body, doesn’t it make sense to first and foremost maintain this healing process the way God intended—not by drugs developed by scientists for a substantial profit?
To naturally induce autophagy as we age, it is essential to make intentional lifestyle choices, such as intermittent fasting, regular exercise, and, for example, maintaining a ketogenic diet. Likewise, other strategies include varying body temperature. For instance, saunas and cold plunges can stimulate autophagy. Achieving 7 to 8 hours of quality sleep each night can also help, as autophagy is known to occur during sleep. The simplest way to stimulate autophagy in your body is by incorporating fasting (such as intermittent fasting, where you fast for 16 hours and eat for 8 hours) and regular exercise into your routine. Trust your instincts, do your own research, and learn to use your body’s incredible natural resources to thrive.








